Chronic back pain is one of the most common and debilitating conditions affecting millions of people worldwide. For those who have struggled with back pain for months or even years, finding a long-lasting solution can be life-changing. One such treatment option is a permanent nerve block for back pain, which can provide significant relief for individuals who haven’t found success with traditional therapies. In this article, we will explore what a permanent nerve block is, how it works, the benefits and risks, and who may benefit from this procedure.
What is a Permanent Nerve Block for Back Pain?
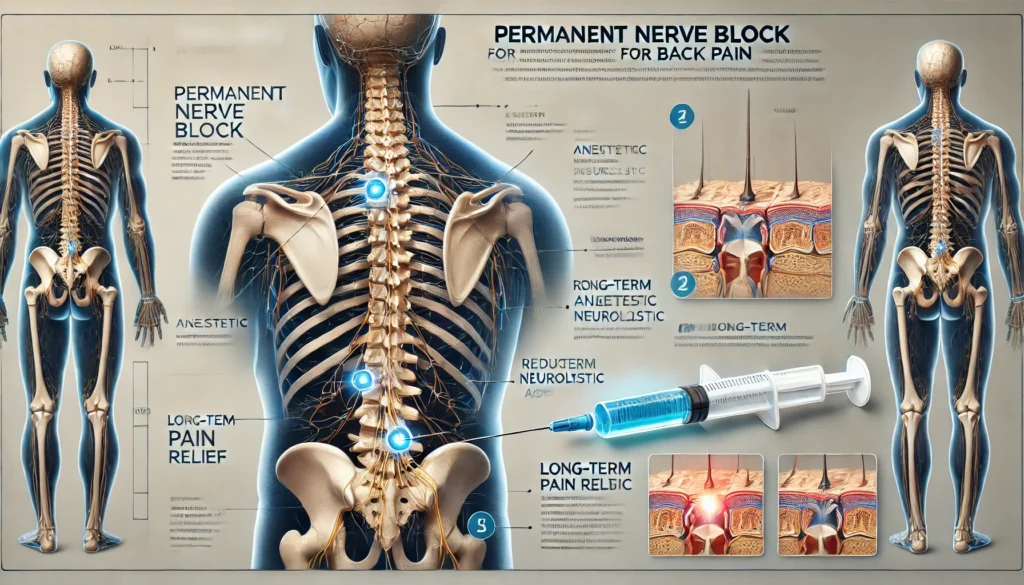
A permanent nerve block is a minimally invasive procedure designed to alleviate chronic back pain by disrupting the nerve signals responsible for transmitting pain. This procedure targets the nerves that are causing pain in the back or related areas, such as the legs. By blocking these pain signals, a nerve block can provide long-lasting pain relief, often with a significant improvement in mobility and quality of life.
Unlike temporary nerve blocks that provide short-term relief, a permanent nerve block involves the use of specialized techniques or medications that aim to provide long-term or even permanent relief from back pain. This can be an ideal solution for individuals with conditions like herniated discs, sciatica, or spinal stenosis.
Read Also: Back Pain Chart – Types of Back Pain: A Visual Guide with Back Pain Charts!
How Does a Permanent Nerve Block Work?
The procedure for a permanent nerve block involves injecting a local anesthetic or using radiofrequency ablation (RFA) to target the pain-causing nerves in the affected area of the spine. The goal is to interrupt the pain signals before they reach the brain. There are different types of nerve block procedures, but most permanent nerve blocks involve one of the following techniques:
- Radiofrequency Ablation (RFA):
This is a technique in which heat is used to destroy nerve tissue. The heat disrupts the nerve’s ability to transmit pain signals, providing long-lasting relief. RFA is often used for facet joint pain or for nerves that are responsible for chronic pain in the lower back or neck. - Chemical Neurolysis:
In this procedure, a chemical solution is injected around the nerves to destroy or block the transmission of pain signals. The effect can last for months or even years, depending on the individual and the specific nerve targeted. - Epidural Steroid Injections:
While not always permanent, epidural steroid injections can provide relief by reducing inflammation around the nerve roots. If successful, the effects may last for months or longer.
Benefits of Permanent Nerve Blocks for Back Pain
- Long-lasting Pain Relief
One of the most significant benefits of a permanent nerve block is its ability to provide long-term pain relief. Patients may experience relief for months or even years, significantly improving their quality of life. - Minimally Invasive
Permanent nerve block procedures are minimally invasive, meaning they require only small incisions or needle injections. This results in less risk of complications, a shorter recovery time, and less discomfort compared to traditional surgery. - Improved Mobility and Function
By reducing or eliminating back pain, patients can regain mobility and perform everyday activities with less difficulty. This improvement can lead to a more active lifestyle and better overall health. - Alternative to Surgery
For individuals who are not candidates for surgery or prefer to avoid it, permanent nerve blocks can offer an effective alternative. It is a less invasive approach that can provide significant relief without the risks and recovery associated with surgery. - Low Risk of Complications
Since the procedure is minimally invasive, the risk of complications is generally low. Most patients experience only mild soreness or discomfort after the procedure, which resolves quickly.
Who is a Good Candidate for a Permanent Nerve Block?
A permanent nerve block is typically recommended for individuals who have chronic back pain that has not responded well to other treatments, such as physical therapy, medications, or traditional injections. Some conditions that may make a person a good candidate for a nerve block include:
- Herniated Discs: When a disc in the spine bulges and compresses nearby nerves, causing pain.
- Spinal Stenosis: Narrowing of the spinal canal, which can put pressure on the nerves and cause pain.
- Facet Joint Dysfunction: Pain originating from the joints in the spine that can affect movement and flexibility.
- Sciatica: Pain that radiates down the leg, often caused by pressure on the sciatic nerve from a herniated disc or other spinal conditions.
- Failed Back Surgery Syndrome: Chronic pain that persists after back surgery, where nerve blocks can provide pain relief when other treatments fail.
Before deciding on a permanent nerve block, a thorough evaluation by a healthcare provider is necessary to determine if the procedure is appropriate for your specific condition.
What to Expect During and After the Procedure
During the Procedure
A permanent nerve block is typically done as an outpatient procedure. The process may include:
- Local anesthesia to numb the area where the procedure will be performed.
- A fluoroscope (a type of X-ray) to guide the doctor in precisely placing the needle or catheter.
- Injection of medication or use of radiofrequency to target the affected nerves.
Most procedures take between 30 minutes to an hour, depending on the complexity of the case.
After the Procedure
Recovery from a permanent nerve block is generally quick. Most people experience only mild soreness in the area where the needle was inserted, and this discomfort usually subsides within a few days. Pain relief may begin immediately, but it can take a few weeks for the full effects to be felt.
Patients can usually resume normal activities within a few days, although they should avoid heavy lifting or intense physical activity during the initial recovery period. Regular follow-up appointments will help monitor progress and ensure the effectiveness of the treatment.
Risks and Considerations
While a permanent nerve block is generally safe, like any medical procedure, there are some risks involved:
- Infection: As with any injection, there is a small risk of infection at the injection site.
- Nerve Damage: In rare cases, the procedure can inadvertently cause damage to the nerves.
- Temporary Pain Flare: Some patients may experience a temporary increase in pain after the procedure, although this usually resolves within a few days.
- Not Effective for Everyone: While many patients experience significant pain relief, nerve blocks may not work for everyone, and the procedure may need to be repeated in some cases.
FAQs:
1 What is a permanent nerve block for back pain?
A permanent nerve block is a procedure that disrupts nerve signals to provide long-term pain relief for chronic back pain.
2 How long does a permanent nerve block last?
The effects can last for several months to years, depending on the type of nerve block and individual response.
3 Is a permanent nerve block a safe procedure?
Yes, it is generally safe with minimal risks, but like any procedure, it carries a small risk of complications.
4 Who is a good candidate for a permanent nerve block?
Individuals with chronic back pain, herniated discs, sciatica, or spinal stenosis who haven’t found relief from other treatments may benefit.
5 How long does recovery take after the procedure?
Most patients recover within a few days, though they should avoid heavy physical activities during the initial recovery period.
Conclusion:
A permanent nerve block for back pain can be a highly effective treatment for those struggling with chronic back pain that hasn’t responded to other treatments. By targeting the nerves that transmit pain, this minimally invasive procedure can offer long-lasting relief and significantly improve quality of life. While not suitable for everyone, it provides a valuable alternative to surgery and can be an excellent solution for many individuals. If you’re considering a permanent nerve block, consult with your healthcare provider to determine if it’s the right option for your specific condition.