Hernias are a common health issue that affects many people worldwide. They occur when an internal organ or tissue pushes through a weak spot or opening in the muscle or surrounding tissue. While hernias are typically associated with visible bulges in the abdomen or groin area, can a hernia cause back pain as well? In this article, we’ll explore the relationship between hernias and back pain, their causes, symptoms, and what you can do to manage both conditions effectively.
What Is a Hernia?
Before understanding how a hernia can cause back pain, it’s important to first define what a hernia is. A hernia occurs when an organ, tissue, or fatty part of the body protrudes through a weak spot or opening in the surrounding muscle or connective tissue. Hernias commonly affect areas like the abdomen, groin, and diaphragm, but they can occur anywhere in the body.
The most common types of hernias include:
- Inguinal Hernia: Occurs in the groin area, affecting both men and women.
- Hiatal Hernia: Happens when part of the stomach pushes up into the diaphragm.
- Umbilical Hernia: Appears near the belly button, often seen in infants or pregnant women.
- Incisional Hernia: Forms at the site of a previous surgical incision.
- Femoral Hernia: Occurs in the upper thigh, more common in women.
While these hernias typically cause discomfort in the affected area, they can sometimes lead to referred pain in other regions of the body, including the back.
Read Also: Can a Hernia Cause Back Pain Female – Is it possible for a hernia to trigger back pain in females!
Can a Hernia Cause Back Pain?
Yes, a hernia can potentially cause back pain. Although back pain isn’t the most common symptom of a hernia, it can occur under certain circumstances, particularly with inguinal hernias, lumbar hernias, or hiatal hernias. The underlying cause of this pain often stems from the pressure or strain placed on the surrounding tissues, nerves, and muscles.
Here are some ways in which a hernia can contribute to back pain:
Inguinal Hernia and Nerve Compression
Inguinal hernias occur when part of the intestine pushes through the abdominal wall or into the groin. This can sometimes affect nearby nerves, causing pain that radiates to the lower back or pelvic region. The muscles in the lower back may also become strained as they try to compensate for the weakened area in the abdominal wall.
Lumbar Hernia and Spine Pressure
A lumbar hernia occurs in the lower back or spine, and it can cause direct pressure on the spinal nerves. This pressure can lead to shooting pain, stiffness, or numbness in the lower back, often mimicking sciatica or a herniated disc. The pain can worsen with movement or activities that stress the back.
Hiatal Hernia and Referred Pain
Although a hiatal hernia primarily affects the upper abdomen, it can sometimes cause referred pain that extends to the back. The discomfort typically arises from the pressure exerted by the stomach on the diaphragm and other surrounding muscles. This pressure can lead to muscle tension, which may manifest as upper or mid-back pain.
Symptoms of a Hernia that May Lead to Back Pain
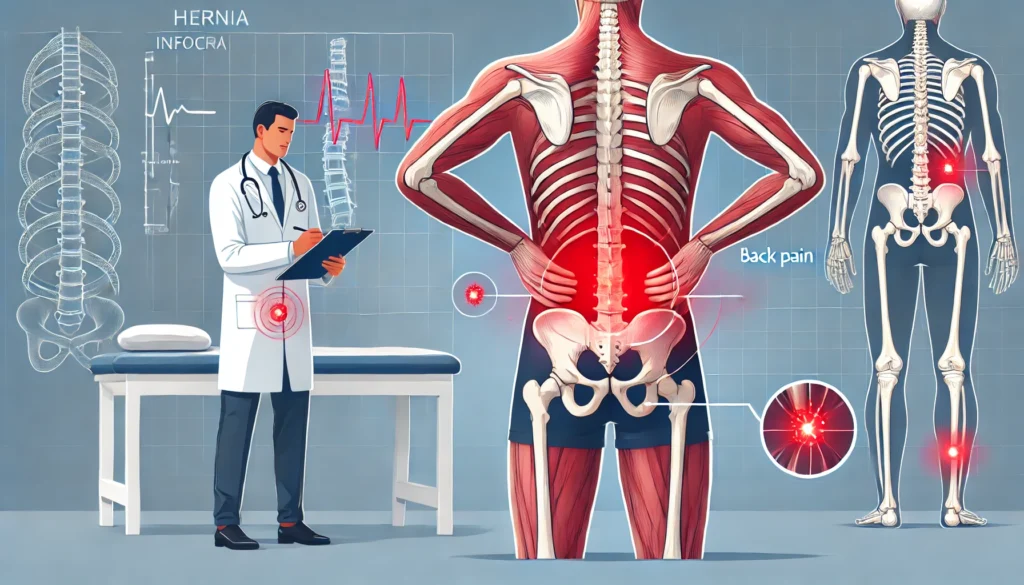
If you are experiencing back pain along with other signs, you may have a hernia. Here are some common symptoms of a hernia that could point to a back-related issue:
- Visible bulge or swelling: A noticeable bulge in the abdomen or groin area may be the first sign of a hernia.
- Pain or discomfort: You may feel pain or tenderness around the bulging area, and it can radiate to the back, particularly with movement.
- Weakness or heaviness: Hernias often lead to a sensation of weakness or heaviness in the affected area, which can strain the back muscles.
- Nausea or vomiting: In severe cases, a hernia can obstruct the intestines, leading to nausea, vomiting, and abdominal pain, which could be accompanied by back pain due to the strain on the body.
How to Manage Back Pain Caused by a Hernia
If you suspect your back pain is related to a hernia, it’s crucial to seek medical advice for an accurate diagnosis and appropriate treatment plan. Here are some strategies to manage back pain associated with a hernia:
Rest and Avoid Strenuous Activity
When dealing with a hernia, it’s important to rest and avoid activities that could exacerbate the condition, such as heavy lifting or bending. Overexertion can strain the abdominal muscles and worsen the pain in your back.
Physical Therapy and Exercises
In some cases, physical therapy can be beneficial for managing back pain caused by a hernia. A physical therapist can guide you through exercises that strengthen the muscles surrounding the hernia and alleviate pressure on the spine and nerves.
Pain Relief Medication
Over-the-counter pain relief medications, such as ibuprofen or acetaminophen, can help manage the pain associated with a hernia. In more severe cases, a doctor may prescribe stronger pain medications or recommend a corticosteroid injection to reduce inflammation.
Hernia Surgery
In some cases, surgery may be necessary to repair the hernia. This is typically recommended if the hernia is causing significant pain, complications, or interference with daily activities. Surgery can also help alleviate back pain that results from nerve compression or muscle weakness.
When to See a Doctor
If you experience any of the following symptoms along with back pain, you should see a doctor promptly:
- Increasing pain or discomfort in the back or affected area.
- Difficulty moving or performing daily tasks due to pain.
- Fever or signs of infection around the hernia.
- Nausea, vomiting, or abdominal bloating, which could indicate a more serious issue like a strangulated hernia.
A healthcare professional will perform a thorough evaluation, including physical exams and imaging tests, to diagnose the issue and recommend the best course of action.
FAQs:
1 Can a hernia cause lower back pain?
Yes, a hernia can cause lower back pain if it affects nerves or muscles in the surrounding area, such as in inguinal or lumbar hernias.
2 What are common hernia symptoms?
Common symptoms of a hernia include visible bulging, pain or tenderness in the affected area, and possible back pain if nerves are compressed.
3 How do you treat back pain from a hernia?
Treatment options include rest, physical therapy, pain relief medications, and in some cases, surgery to repair the hernia.
4 When should I see a doctor for back pain related to a hernia?
See a doctor if the pain worsens, if you have difficulty moving, or if you experience fever, nausea, or vomiting along with back pain.
5 Can a hernia heal without surgery?
While some small hernias may be manageable with non-surgical treatments, surgery is often needed for more severe or complicated hernias to prevent further pain or complications.
Conclusion:
While back pain is not the most common symptom of a hernia, it is possible for a hernia to cause discomfort or pain in the back, especially in cases involving nerve compression or pressure on the surrounding tissues. If you’re experiencing back pain along with other signs of a hernia, it’s essential to seek medical advice to determine the best treatment and alleviate the pain. In many cases, conservative treatments like physical therapy, pain relief, and rest can help, but surgery may be necessary in more severe cases.Always consult with a healthcare provider to address your symptoms and ensure you’re getting the appropriate care for both your hernia and any related back pain.